[ad_1]

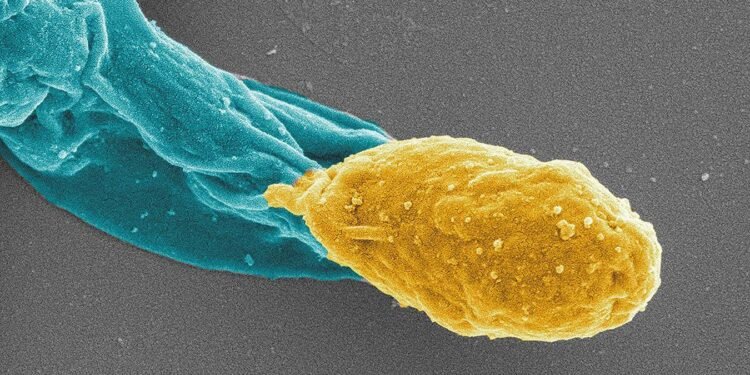
A brand new antibiotic successfully treats Clostridium difficile infections in mice, and likewise helps stop the formation of recent spores (pictured in yellow)
Jeshina Janardhanan and Yuanyuan Qian
A brand new antibiotic is just not solely more practical than our first-line remedies for Clostridium difficile infections, but it surely additionally considerably reduces the danger of reinfection, in line with research in mice.
C. difficile causes signs together with belly cramping, diarrhoea and fever, and in excessive instances extreme dehydration and kidney failure. Such infections kill about 13,000 folks yearly within the US alone.
For that cause, it’s one in all 5 antibiotic-resistant infections presently listed by the US Facilities for Illness Management and Prevention (CDC) as “urgent threats”, however its deadliness is admittedly in a category of its personal.
“Clostridium difficile an infection leads to greater than seven instances the deaths because the remaining 4 CDC pressing threats mixed,” says Mayland Chang on the College of Notre Dame in Indiana and lead writer of the examine figuring out the brand new antibiotic.
C. difficile infects the intestine, typically after folks have taken antibiotics to clear one other an infection. That may eradicate their intestine microbiome, permitting C. difficile to take up residence, typically when folks inhale airborne spores within the hospital.
The primary-line antibiotic, vancomycin, works effectively for preliminary infections, however turns into much less efficient thereafter.
“Vancomycin has no exercise in opposition to spores, and recurrence of C. difficile an infection after a course of vancomycin stays a giant downside,” says Alexander Khoruts on the College of Minnesota.
Meaning the micro organism’s spores can reside silently within the physique and trigger an infection years down the road. About 25 per cent of individuals contaminated with C. difficile will go on to have a second an infection, says Chang. Forty per cent of people that have a second an infection may have a 3rd, and 65 per cent who’ve a 3rd an infection may have a fourth, she says.
She and her group sought to interrupt the reinfection cycle. They searched a database of anti-bacterial molecules, screening for compounds with exercise in opposition to a particular form of binding protein in micro organism. This led them to 2 compounds: oxadiazole 1 and oxadiazole 2. In in vitro exams, each compounds killed C. difficile when utilized at the identical concentrations as vancomycin.
Oxadiazoles are quickly absorbed into the bloodstream. However for intestine infections that could be a downside – the drug wants to remain within the intestine. Oxadiazole 2 quickly exited into the blood of mice, so the staff didn’t pursue it additional. Oxadiazole 1, nevertheless, stayed put. In a collection of C. difficile an infection research, oxadiazole 1 protected mice from demise about 30 per cent higher than vancomycin. Contaminated mice that bought oxadiazole 1 regained misplaced weight inside three to 5 days, the place vancomycin-treated mice had been nonetheless underweight for weeks after preliminary an infection.
However maybe probably the most promising outcome was to the best way the drug halted persistent infections. Oxadiazole 1 blocks two C. difficile proteins that assist the micro organism type drug-resistant spores. After three weeks of remedy, mice receiving vancomycin nonetheless had detectable spores of their faeces and went on to have recurring infections. Mice handled with oxadiazole 1 had no quantifiable spores and had no reinfections throughout the examine interval.
The findings might trace at a brand new solution to deal with C. diff infections in folks. One other remedy that has proven promise is faecal microbiota transplants (FMT), the place folks obtain stool from an uninfected donor to be able to re-establish a wholesome intestine microbiome. Two commercially out there FMT-based medicine had been not too long ago accredited by the Meals and Drug Administration, however these aren’t at all times efficient.
“We completely want new drug growth” for treating C. difficile, says Khoruts.
Matters:
[ad_2]
Source link